Imagine you are a new Physician working in a group practice as part of an Academic Medical Center (AMC). You may be surprised to learn that you are soon expected to play a leading role in managing the day-to-day process flows of the clinic. This may sound strange since you are the newest member of the group. But it is not really surprising. Most Attendings want to leave day to day operations behind and focus on other matters, including research, patient care, and outside interests. You may ask yourself a simple question like, “Is the appointment schedule that we use the best we can do?”
The clinic has been operating for quite some time before you came along and a schedule has evolved based on common templates, trial and error, and random adjustments. You may want to know how the performance of the system will change if you make a change such as, adding an examination room, double-booking patients at the start of the day, or staggering the start times of the Attendings in the clinic. These, and a myriad of similar questions are each extremely difficult to answer using mathematical theory, or optimization models for a variety of reasons.
Mathematical models used in optimization depend on making a set of assumptions about process flows and activity times that are not easy to justify in healthcare settings. Many statistical models assume that the variables of interest are independent and identically distributed (i.i.d.). Such assumptions are invalid in clinic settings for a variety of reasons. Activity times for new patients have a different distribution when compared to returning patients. Activity times for trainees such as Residents or Fellows differ from those of Attending Physicians (Attendings). In addition, we have found that activity times differ when the status of the system changes over time. This fact violates the assumption of virtually all optimization or queueing models.
What’s a simulation?
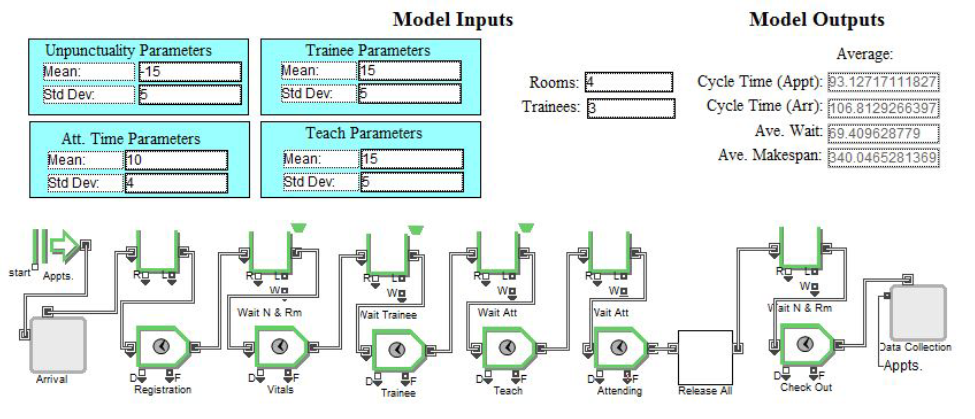
Fortunately, there is a “quick and dirty” way to address such problems that can accommodate many idiosyncrasies of health care settings. You can create a numerical representation of the clinic setting and use it as a grounds for experimentation as you consider process changes. This is known as the use of Discrete Event Simulation (DES). Its called Discrete Event simulation because the start and/or end of a process step can be thought of as discrete events, even though the time between these points in time come from a continuous distribution. What is needed to build such as model is a detailed description of the process flows, the resources involved, and the activity times observed. We emphasize the term “observed” here because standard times, or data available in most information systems has repeatedly proven to be significantly different from reality. As an example of a simple DES model consider the schematic shown below.
What do I do with this?
This process reflects a setting in which patients arrive according to an appointment schedule, with some added “Unpunctuality.” Unpunctuality is simply the random deviation from the schedule, or the gap between the appointment time and the arrival time. The patient checking in (Registration), is led by a nurse to the examination room where basic information is collected. In this diagram, we are labeling this step (Vitals). The Resident then interacts with the patient (Trainee). After leaving the exam room the Resident discusses the case with the Attending (Teach). The Attending and Resident then revisit the patient together (Attending). The patient then dresses and visits the front desk before leaving the clinic (Check Out). Adjustment of multiple model parameters (in the Blue blocks) allows us to reshape the distributions for Unpunctuality, along with a number of activity times. This model also allows us to change the number of Examination Rooms (Rooms) and Residents (Trainees). We have used this particular model in multiple studies. The general approach is to simulate as many sessions as we like and use insights provided about a number of critical metrics such as:
- Cycle time – Appt (Time from Appointment time to exit)
- Cycle time – Arr (Time from Arrival time to exit)
- Ave Wait (Average time in the waiting room before entry to the examination room)
- Ave Makespan (Time from entry of first patient on the schedule to exit of the last)
We have created a number of models of this style and used them to address a host of questions in a variety of settings including:
- How does patient tardiness alter clinic performance? (See Williams et.al. 2014)
- How does including Resident education alter capacity and cycle times? (See Williams et.al. 2012
- How do we use simulation data to help assess costs and service value? ( See Elnahal, et.al. 2015)
- What happens when Attendings change activity times based on clinic status? (See Chambers, et.al. 2016)
- What happens when we move some educational activities outside of clinic hours? (See Williams, et.al. 2016
Take Away’s
Many service settings include a host of nuances based on both customers and providers. This make simple approximations or models unreliable predictors of system behavior. In these instances a flexible tool like Discrete Event Simulation can be quite helpful. We have used this tool to work with a number of clinics in areas including Dermatology, Obstetrics, Orthopedics, Pain Management, Physical Medicine and Rehabilitation, and Outpatient Surgery. Details about much of this work can be found in the scholarly papers housed on our Documents page as well as our text at, Amazon.com.
Testy, test, test!!!